Introducing Thrive's clinical advisory board.
At Thrive, we believe clinical excellence isn’t built in isolation. It grows in community—with those who inspire, challenge, and stretch us to become better. Our Clinical Advisory Board exists to do just that.
A living library of wisdom. A circle of Trusted Guides.
This isn’t just a list of names on a page. It’s a gathering of pioneers—warm-hearted scholars, seasoned clinicians, visionary advocates, and trusted medical providers—who’ve dedicated their lives to transforming mental health care. Together, they bring deep expertise in anxiety and OCD treatment, eating disorder recovery, pediatric and adolescent psychiatry, adult mental health, and systemic change in care delivery.

Obsessive Compulsive Disorder

Perinatal
Mental Health
Obsessive Compulsive Disorder
Perinatal
Mental Health
Advisory Board Members and Consultants
Meet our heroes
Eric Alan Storch, Ph.D.
Clinical Advisory Board Member
Eric Storch, Ph.D. is Professor and McIngvale Presidential Endowed Chair in the Department of Psychiatry and Behavioral Sciences at Baylor College of Medicine (BCM). He serves as Vice Chair and Head of Psychology, and co-directs the Obsessive-Compulsive and Related Disorders program at BCM. Dr. Storch specializes in the nature and treatment of childhood and adult obsessive-compulsive disorder, anxiety disorders, PTSD, and anxiety among youth with autism. In addition to over 850 published articles and chapters and 24 books, he has received multiple federal grants to investigate treatment efficacy, mechanisms of action, genetics, bioethics, innovative approaches to phenotyping, and how to enhance outcomes for those struggling with OCD and related conditions.
“I joined the advisory board because I believe Thrive is setting a new standard for adolescent eating disorder care—one that honors both families and evidence-based practice.”
Stephanie Woodard, Psy.D.
Clinical Advisory Board Member
Stephanie Woodard, Psy.D. is a licensed psychologist and systems-level strategist specializing in population health and translating research into policy and practice. She previously served as Nevada’s state mental health and substance use authority, leading statewide initiatives on crisis services, opioid settlement funding, Medicaid expansion for substance use treatment, and harm reduction access. Dr. Woodard has contributed to national training and technical assistance efforts, taught at the University of Nevada, and focused her clinical work on co-occurring disorders, mindfulness-based cognitive therapies, and positive psychology. Her leadership roles include service on the Nevada Board of Psychological Examiners, the Attorney General’s Substance Use Working Group, and national behavioral health associations. She has been recognized with the Robert Rehmar Professional Award and the Distinguished Speaker Award from the National Latino Behavioral Health Association.
“I joined the advisory board because I believe Thrive is setting a new standard for adolescent eating disorder care—one that honors both families and evidence-based practice.”
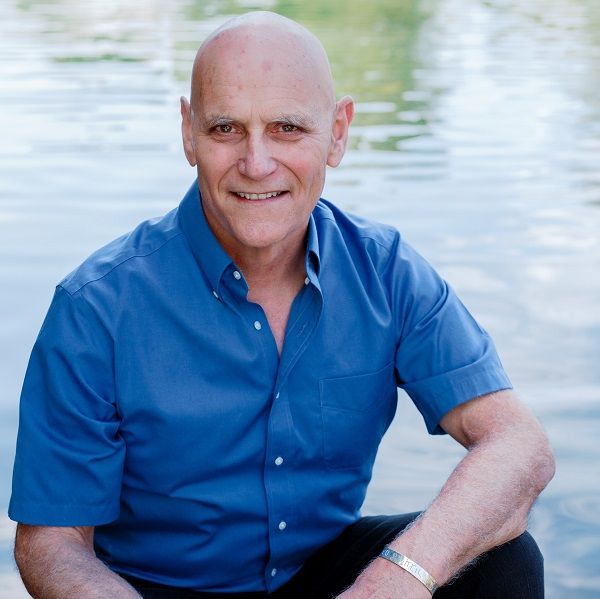
Steven C. Hayes, PhD
Clinical Advisory Board Member
Steven C. Hayes, Ph.D. is Emeritus Professor of Psychology at the University of Nevada, Reno, and President of the Institute for Better Health. He is best known as the originator of Acceptance and Commitment Therapy (ACT), Relational Frame Theory (RFT), and the Psychological Flexibility Model, as well as co-developer of Prosocial and Process-Based Therapy. His work has advanced Contextual Behavioral Science, functional contextualism, and evolutionary approaches to human cooperation and well-being. Dr. Hayes has authored 47 books and nearly 700 scientific articles, making him one of the most cited psychologists in the world, and has received numerous honors including the Lifetime Achievement Award from the Association for Behavioral and Cognitive Therapies and the Impact of Science on Application Award from the Society for the Advancement of Behavior Analysis.
“I joined the advisory board because Thrive is helping to create a new more personalized way forward for evidence-based care in which the whole person truly is the focus.”

Carolyn Costin
Consultant
Carolyn Costin, MA, MEd., MFT, CEDS, FAED, is a globally recognized eating disorder clinician, author, and speaker. After recovering from anorexia, she pioneered the belief that full recovery is possible and founded Monte Nido, the first residential program in a home setting combining clinical care with holistic practices. She has authored six books, trained professionals worldwide, and served in leadership roles across major eating disorder organizations. In 2016, she launched The Carolyn Costin Institute to train coaches, provide clinical education, and advance the field through speaking and consultation.
Though not a member of our clinical advisory board, Carolyn plays a vital role at Thrive as a trusted clinical consultant, offering her expertise to help shape our programs and guide our approach.
Fill your guts, or spill your guts.
At Thrive, we believe it’s important to not always be so serious in the clinical world. This video is proof. Thrive Wellness founder Kat Geiger challenges psychologist Dr. Eric Storch to a hilarious round of ‘Spill Your Guts or Fill Your Guts,’ where awkward questions meet bizarre foods — all in the name of exposure therapy (and a good laugh).
Start your healing journey today
NEXT STEPS
Are you ready to find hope? We can't wait to connect you with the care you need. To get started with us, please reach out using the link below.

Obsessive Compulsive Disorder

Perinatal
Mental Health
Obsessive Compulsive Disorder
Perinatal
Mental Health
Our Latest Posts: