Finding Food Freedom Through Intuitive Eating and Mindful Eating

By Thrive’s National Director of Nutrition Services Kailey Cunningham, M.S., RDN, CD
WHAT IS INTUITIVE EATING?
Intuitive Eating is a non-diet approach to health developed in 1995 by two dietitians, Evelyn Tribole, MS, RDN, CEDRD-S, and Elyse Resch, MS, RDN, CEDRD-S, FADA, FAND. The holistic framework focuses on internal cues rather than external rules to help guide eating and movement choices. Intuitive Eating promotes eating in a way that works best for the body and brain while honoring both physical and mental health. The ultimate goal is to cultivate a more peaceful and healthy relationship with both food and the body.
IntuitiveEating.org describes Intuitive Eating as “a self-care eating framework, which integrates instinct, emotion, and rational thought…Intuitive Eating is a weight-inclusive, evidence-based model with a validated assessment scale and over 100 studies to date.” Intuitive Eating challenges the idea that there is a “right” way to eat. Instead, it asks individuals to use their experiences and sensations to guide their eating. In doing so, they can learn to trust their bodies and brains to communicate what they need.
The framework is sometimes oversimplified and misunderstood as eating whatever you want whenever you want. While it’s true that unconditional permission to eat is a key part of eating intuitively, the approach is more complicated than that.
The 10 Principles of Intuitive Eating can provide more insight into the nuances of the approach. They are as follows:
- Reject the diet mentality.
- Honor your hunger.
- Make peace with food.
- Challenge the food police.
- Discover the satisfaction factor.
- Feel your fullness.
- Cope with your emotions with kindness.
- Respect your body.
- Movement-Feel the difference.
- Honor your health with gentle nutrition.
Moving through the principles looks different for each individual based on their past experiences and current level of connection with their body’s cues. For most folks, dismantling diet culture-influenced thoughts takes time. As such, becoming an intuitive eater is a journey that requires patience, exploration, and experimentation.
The Benefits of Intuitive Eating
Ultimately, Intuitive Eating helps eliminate food rules and encourages individuals to trust their bodies to guide their eating choices. When a person implements Intuitive Eating, they no longer need someone else to tell them when, what, or how much to eat. Instead, they can listen to their internal cues in combination with observations from their past eating experiences. By connecting the mind, body, and spirit, Intuitive Eating allows individuals to eat in ways that feel good while empowering them with confidence and autonomy to make authentic eating and movement choices.
Intuitive Eating and Eating Disorders
When individuals with eating disorders move through the process of nutrition rehabilitation and begin implementing the principles of Intuitive Eating, many of the medical and mental health complications brought on by disordered eating begin to resolve. As individuals honor their body’s internal cues, physical symptoms associated with eating disorders, such as gastrointestinal upset, cold intolerance, sleep disturbances, and dizziness start to subside. Likewise, mental health symptoms, such as obsessive thoughts about food, anxiety, and depression also improve. For individuals with eating disorders, Intuitive Eating can be a vital step in learning to nourish their entire well-being.
WHAT IS MINDFUL EATING?
Mindful eating applies the principles of mindfulness to eating experiences. Mindfulness is a form of meditation that focuses on being present without judgment or interpretation. By practicing awareness and acceptance, mindfulness allows individuals to notice their thoughts, feelings, and sensations objectively without needing to take action.
Similarly, mindful eating asks individuals to focus on the experience of food without judgment or worrying about what’s in the food. When a person eats mindfully, their intention is to savor their eating experience by embracing the present moment. This involves using their senses to notice the food’s taste, texture, and temperature, in addition to being aware of how their other senses such as smell, sight, sound, and touch impact their experience.
You can embrace mindful eating by practicing the following:
- Non-judgment: Build awareness of your experience while challenging any moral or other judgments about food. Do your best to avoid labeling foods as “good” or “bad.”
- Acceptance: Be willing to notice what’s happening and accept it rather than trying to change it.
- Letting go: Release past expectations and attachments to food.
- Non-striving: Don’t attach an outcome to your experience. For example, don’t attach a weight goal to your eating experience.
- Trust: Foster awareness of your experience to begin to trust yourself.
- Patience: Know that staying present moment-to-moment is a practice and improvement takes time, so remain patient with yourself.
- Gratitude: Recognize and appreciate that food is fuel that nourishes your body and mind.
You can also try The Three T’s exercise. During the first three bites of a meal or snack, notice the food’s taste, texture, and temperature — or “the three T’s”. In doing so, you’ll create more space for mindfulness throughout your eating experience as well as begin to form a mindfulness habit.
The Benefits of Mindful Eating
By allowing their experiences to guide eating choices, individuals can leave behind any unhelpful, unsustainable, and harmful rules about eating.
Additionally, mindful eating tends to foster more feelings of satisfaction from food. By noticing the flavors, textures, and other sensations involved, a person is more likely to feel satiated until their next eating experience.
Furthermore, mindful eating helps individuals discover their true food preferences. Instead of eating a food because they believe they “should” or eating a food with judgment because they believe they “shouldn’t,” a person can notice what they prefer and don’t prefer about certain foods. Mindful eating allows individuals to experiment with their food preferences as they gather information that will inform future eating experiences. In other words, focusing on the present while eating can help non-judgmentally shape the future.
Mindful Eating and Eating Disorders
During some phases or times of eating disorder recovery, practicing mindfulness can actually create a barrier to eating, due to the severity of thoughts and judgments stemming from the eating disorder. Avoiding mindfulness, however, can keep an individual who is struggling with an eating disorder from noticing any pleasant sensations or acknowledging their experiences while eating. If you’re currently experiencing an eating disorder, discussing the topic of mindful eating with your treatment team is necessary to determine what approach corresponds best to your phase of recovery.
MINDFUL EATING VS. INTUITIVE EATING
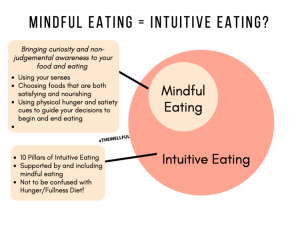
Image Source: The Wellful | 3 Ways to Improve Your Relationship with Food
Mindful eating is an element of Intuitive Eating, so there’s significant overlap between the two. In order to truly be in tune with the body, it’s necessary to be present and aware before, during, and after eating experiences.
Some differences between mindful eating and Intuitive Eating come to light, however, when we consider the logistics of eating. While practicing mindful eating can benefit individuals’ relationships with food as well as their overall mental and physical health, it’s not realistic to practice mindfulness during every meal and snack. For this reason, implementing mindfulness during each eating experience isn’t required by Intuitive Eating. Instead, Intuitive Eating uses other principles to help guide individuals when mindfulness isn’t accessible.
DIET CULTURE’S INFLUENCE ON MINDFUL EATING AND INTUITIVE EATING
The diet industry has created confusion around mindful eating, often suggesting mindfulness as a way to control eating habits rather than foster a healthy mind-body connection. The same argument falsely claims that eating mindfully promotes eating less and subsequent weight loss. While weight change may be a natural side effect that some people experience when they heal their relationships with food, twisting mindfulness into a weight-loss tactic is an example of the ways the diet industry causes harm. Similarly, the diet industry has muddled the concept of Intuitive Eating by promoting it as a weight-loss strategy as well. Any resource touting mindful or Intuitive Eating as a way to promote weight loss doesn’t apply the true principles of either practice and should be avoided.
LEARN MORE ABOUT INTUITIVE EATING AND MINDFUL EATING
To gain a fuller understanding of mindful eating and Intuitive Eating, exploring the 10 principles of Intuitive Eating more thoroughly and experimenting with the application of each principle can be an impactful way to begin your journey. Because mindfulness is a part of Intuitive Eating, you’ll also learn about mindful eating as you move through the principles. To dive even deeper into Intuitive Eating and mindful eating, consider reading Intuitive Eating, 4th Edition and The Intuitive Eating Workbook by Evelyn Tribole, MS, RDN and Elyse Resch, MS, RDN.
GUIDANCE FOR INTUITIVE EATING AND MINDFUL EATING AT THRIVE
Thrive implements both Intuitive Eating and mindful eating into our nutrition philosophy to help our clients heal their relationships with food and their bodies. To learn more about our therapeutic services , nutrition support, and eating disorder treatment programs , please reach out .
About the Author
Thrive Wellness’s National Director of Nutrition Services Kailey Cunningham, MS, RDN, CD
Kailey Cunningham, MS, RDN, CD, is a Registered Dietitian Nutritionist who obtained a Master’s of Dietetics degree from the University of Kentucky after completing both her undergraduate studies in dietetics and accredited dietetic internship at the same university.
She has been a Registered Dietitian Nutritionist since February of 2013 and has been working in the eating disorder field since 2015. Kailey has experience treating clients at many levels of care, from partial hospitalization programming to outpatient, with a variety of diagnoses including anorexia nervosa, bulimia nervosa, binge eating disorder, ARFID and OSFED.
She began working at The Emily Program in Washington for three years where she acted as the full-time programming dietitian. While in this position, she worked directly with a lead therapist to develop an adolescent treatment track implementing elements of Family-Based Treatment and gaining invaluable experience working with adolescents and their parents. She then worked at Center for Discovery while building her nutrition counseling private practice. She began her successful practice in April of 2018 and moved it with her from Olympia, Washington to Rocklin, California in October 2020. Kailey is excited to now be a part of the Thrive Wellness team.
Kailey’s primary motivator and true passion is supporting others on their journey to a more peaceful and balanced relationship with food and their bodies. Through individualized nutrition counseling and education, she helps those struggling with eating disorder behaviors, body image issues, food aversion and health anxieties find what is right for them while leaving diet culture behind.
The post Finding Food Freedom Through Intuitive Eating and Mindful Eating first appeared on Thrive Wellness.








